Complications of Pregnancy
What are some of the more common complications of pregnancy?
Most pregnancies are uneventful. But sometimes complications happen. Here are some of the more common pregnancy complications.
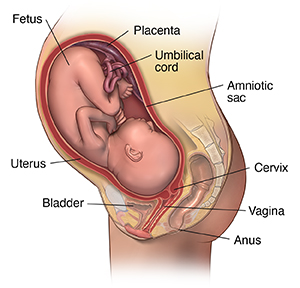
Amniotic fluid complications
Too much or too little amniotic fluid in the sac around the fetus may be a sign of a problem with the pregnancy. Too much fluid can put too much pressure on the pregnant person's uterus, leading to preterm labor. It also can cause pressure on the pregnant person's diaphragm. This can cause problems breathing. Fluids tend to build up in cases of uncontrolled diabetes, a multiple pregnancy, incompatible blood types, or birth defects. Too little fluid may be a sign of birth defects, growth retardation, or stillbirth.
Bleeding
Bleeding in late pregnancy may be a sign of a placental problem, a vaginal or cervical infection, or preterm labor. Women who bleed in late pregnancy may be at greater risk of losing the fetus and bleeding a lot. Tell your healthcare provider right away if you have bleeding at any time during the pregnancy.
Ectopic pregnancy
An ectopic pregnancy is when the fetus develops outside of the uterus. This can happen in the fallopian tubes, cervical canal, or the pelvic or belly. The cause of an ectopic pregnancy is often scar tissue in the fallopian tube from infection or disease. The risk of ectopic pregnancy is higher in people who have had tubal sterilization procedures, especially people who were younger than age 30 at the time of sterilization.
Ectopic pregnancies happen in about 1 out of 50 pregnancies. They can be very unsafe for the pregnant person. Symptoms may include spotting and cramping. The longer an ectopic pregnancy goes on, the greater the chance that a fallopian tube will rupture. An ultrasound and blood tests may confirm the diagnosis. Treatment of an ectopic pregnancy may include medicine or surgery to take out the fetus.
Miscarriage or fetal loss
A miscarriage is pregnancy loss that happens up to 20 weeks of gestation. Most miscarriages happen before 12 weeks. Miscarriages happen in about 1 in 10 to 3 in 20 pregnancies. They are often due to genetic or chromosomal abnormalities.
Miscarriages are usually preceded by spotting and intense cramping. To confirm a miscarriage, an ultrasound and blood tests may be done. The fetus and contents of the uterus are often naturally expelled. If this does not happen, a procedure called a dilation and curettage (D & C) may be needed. This procedure uses special tools to remove the abnormal pregnancy.
Fetal loss in the second trimester may happen if the cervix is weak and opens too early. This is called incompetent cervix. In some cases, a healthcare provider can help prevent pregnancy loss by stitching the cervix closed until delivery. The hormone progesterone may also be given to stop the cervix from dilating during pregnancy.
Placental complications
In a normal pregnancy, the placenta attaches to the uterine wall. But 3 types of placental complications may happen:
Placental abruption. Sometimes the placenta becomes detached from the uterine wall too soon. This is called placental abruption. It leads to bleeding and less oxygen and nutrients to the fetus. The detachment may be complete or partial. The cause of placental abruption is often unknown. Placental abruption happens in about 1 in every 100 live births.
Placental abruption is more common in women who smoke, have high blood pressure, or have a multiple pregnancy. It also happens in people who have had previous children or a history of placental abruption. Symptoms and treatment depend on the degree of detachment. Symptoms may include bleeding, cramping, and belly tenderness. Diagnosis is often confirmed with a physical exam. An ultrasound may also be done. People are usually put in the hospital for this condition. They may have to deliver the baby early.
Placenta previa. Normally, the placenta is located in the upper part of the uterus. Placenta previa is a condition in which the placenta is attached close to or covering the cervix (the opening into the uterus). This type of placental complication happens in about 1 in every 200 deliveries. It happens more often in people who have scarring of the uterus from past pregnancies. It also happens in people who have fibroids or other problems in the uterus, or in people who have had uterine surgeries.
Symptoms may include vaginal bleeding that is bright red and not linked with belly tenderness or pain. Diagnosis is confirmed by doing a physical exam and an ultrasound. Depending on how bad the problem is and the stage of pregnancy, a change in activities or bed rest may be ordered. The baby often has to be delivered by cesarean section. This keeps the placenta from detaching early and depriving the baby of oxygen during delivery.
Placenta accreta. Sometimes the placenta or part of the placenta invades the uterine wall. This may result in third trimester bleeding. This problem may be found before delivery with ultrasound or MRI. It can lead to life-threatening bleeding. A healthcare provider will plan the delivery carefully. Often, a hysterectomy is needed after delivery.
Preeclampsia or eclampsia
Preeclampsia (or toxemia) causes high blood pressure during pregnancy. Protein is also found in the urine. Sometimes a pregnant person has swelling due to fluid retention. Eclampsia is the more severe form of this problem. It can lead to seizures, coma, or even death.
The cause of preeclampsia is unknown. But it is more common in first pregnancies. It affects about 1 in 20 to 4 in 50 pregnant people. Other risk factors for preeclampsia include:
A person carrying multiple fetuses
A teenage parent
A person older than 40
A person with high blood pressure, diabetes, or kidney disease before they became pregnant
History of thrombophilia or lupus
History of an in vitro pregnancy
A person who is obese with a BMI greater than 30
Symptoms may include severe swelling of the hands and face, high blood pressure, headache, dizziness, irritability, decreased urine output, belly pain, and blurred vision. Treatment will vary based on the severity of the condition and the stage of the pregnancy. Treatment may include a hospital stay, bed rest, medicine to lower blood pressure, and keeping close track of both the fetus and the parent.