Get the facts about cervical cancer
- Category: Women's Health, Obstetrics & Gynecology, Living Well, Cancer Care
- Posted On:
- Written By: Navya Nair, MD

Cervical cancer is cancer that starts in the cervix or the lower portion of the uterus (womb). In 2019, over 13,000 new cases of cervical cancer were diagnosed and over 4,000 women died from cervical cancer in the United States. Before the 1950s, cervical cancer was the most frequent cause of cancer death in women. However, now with the advent of pap smears and screening techniques, the incidence of cervical cancer has gone down. With screening methods, precancerous lesions can be identified and treated before they turn into cancer. In addition, the HPV (human papillomavirus) vaccine can prevent infection from high-risk HPV strains that are key in the development of cervical cancer.
What is cervical cancer?
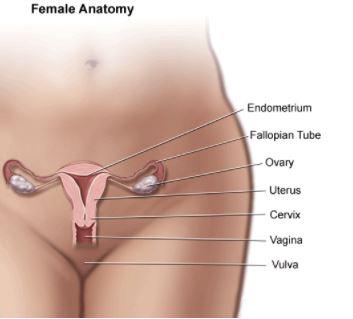
Cervical cancer starts in the cells lining the cervix. The cervix is the lower portion of the uterus (also referred to as uterine cervix). In pregnancy, the uterus is where a fetus grows. The cervix connects the uterus to the vagina (birth canal). The cervix has two components; endocervix and ectocervix. Where the endocervix and ectocervix meet is called the transformation zone. The majority of cervical cancers begin in the transformation zone.
The majority of cervical cancers are squamous cell carcinomas. These begin from cells of the exocervix. The second most common type of cervical cancer is cervical adenocarcinoma. These begin from cells of the endocervix. These two types make up almost all cervical cancers.
What are the symptoms of cervical cancer?
Cervical cancer is usually asymptomatic (no symptoms). This is why it is important to undergo regular screening.
Sometimes, cervical cancer can present with symptoms such as:
- Abnormal vaginal discharge and/or vaginal odor
- Abnormal vaginal bleeding (bleeding after intercourse, bleeding when you are not on your period)
- Pelvic pain or pressure
If these symptoms are present for two weeks or longer, it is important to see a doctor to be evaluated. The CDC offers a gynecologic cancer symptoms diary that can be used to track any symptoms to decide when you need to see your doctor which can be found here.
How does cervical cancer start?
Almost all cervical cancers are caused by the human papillomavirus (HPV). HPV is a virus that can be passed from person to person during sex. There are certain strains of HPV (high-risk HPV) that can lead to cervical precancers and cancers. There are other strains of HPV (low-risk HPV) that can cause genital warts.
HPV is very common that most people are exposed to it in their lifetime. HPV infection is usually asymptomatic so you cannot tell if you have it. Most people clear HPV infections on their own. Some people do not clear the infection, and that can lead to cervical precancers and cancer.
In addition to playing a key role in the development of cervical cancer, HPV is also implicated in cancers of the vulva, vagina, anus, penis, and oropharyngeal cancers.
Risk factors for cervical cancer include:
- Immunosuppression
- HIV infection
- Transplant patients
- Autoimmune disease
- Smoking
- Having several sexual partners
Screening
Dr. George Papanicolaou was a Greek physician who discovered that a smear of cells from the cervix could be used to detect cancer of the cervix. He went on to develop the Pap (Papanicolaou) smear which is a screening test for cervical cancer. In addition to the Pap test, you can also test directly for HPV as a screen. Combined testing or co-testing (Pap test + HPV test) can also be used for screening.
Abnormal screening test results should be evaluated with a diagnostic procedure called a colposcopy where the cervix is visualized with a microscope and biopsies taken. If biopsies show precancerous cells, this can be treated to prevent the development of cervical cancer.
Screening recommendations have changed in recent years from annual Pap smears to less frequently in those with normal testing. While you may not need a Pap smear every year, it is still important to see your gynecologist annually for a full pelvic exam.
HPV Vaccination
The HPV vaccine protects against HPV virus strains that cause cervical, vaginal, and vulvar cancers. All children are recommended to be vaccinated at age 11- 12 years, the vaccine can be given as early as 9 years. The vaccine is also recommended for all people through age 26 years if they have not been vaccinated. The FDA has now approved the vaccine for adults through age 45 years if they have not been previously vaccinated. Adults should speak to their physicians about their risk of new HPV infections and the benefits of vaccination.
If vaccination is done before age 15 years, two doses are recommended 6 – 12 months apart. If vaccination is done after age 15 years, it is recommended to be given in a series of 3 injections. Recent studies have shown that even getting 1 shot can be protective.
In addition to screenings and the HPV Vaccination, you can also reduce your risk of cervical cancer by:
- Avoid smoking
- Use condoms during sex (this does not prevent all HPV infections, but condom use is associated with lower rates of cervical cancer)
- Limit the number of sexual partners

Dr. Navya Nair is a Gynecologic Oncologist at University Medical Center New Orleans and Assistant Professor with LSU Health New Orleans. She studied biomedical engineering also completed a master’s degree in Public Health at Tulane University before moving on to New York University for medical school. She completed her residency in Obstetrics and Gynecology at Emory University in Atlanta and her fellowship in Gynecologic Oncology at Mount Sinai Hospital in New York. Dr. Nair returned to her hometown of New Orleans to practice as a gynecologic oncologist. She specializes in the use of surgery and chemotherapy in treating women with gynecologic cancers. In addition, she is actively involved with the clinical trials program at the Louisiana Cancer Center. Dr. Nair also has a strong interest in global women’s health. She has worked in India, Ethiopia and Liberia and hopes to contribute to improving the care of women worldwide by implementing cancer prevention programs and improving access to cancer care.