Comprehensive Stroke Care at East Jefferson General Hospital
At East Jefferson General Hospital, we are here to help stroke patients
any time—day or night. A stroke is a medical emergency. Every year,
over 795,000 people in the US have a stroke, and many of them are left
with lasting problems causing this to be the leading cause of long-term
disability. With the right care, given at the right time, we can help
people feel better and get back to their lives.
Our hospital works hard to give the best care for stroke. In 2012, we were
named an Advanced Primary Stroke Center. In 2018, we became a Thrombectomy
Capable Stroke Center, which means we added new treatments and more experts
to our team.
In 2024, East Jefferson General Hospital became a
Comprehensive Stroke Center. This is the highest level of stroke care a hospital can have. It means
we can treat even the most serious stroke cases.
East Jefferson General Hospital has also received the American Heart Association/American
Stroke Association’s Get With The Guidelines® Target: Stroke
Gold Plus quality achievement award, which recognizes the hospital’s
commitment to ensuring stroke patients receive the most appropriate treatment
according to nationally recognized, research-based guidelines based on
the latest scientific evidence.
Learn more
2024-2025 Stroke Program Quality Measures and Outcome Data
If your provider has told you that you need expert stroke treatment, we
want you to know that East Jefferson General Hospital is ready to care
for you! Below, you will also find information about how well our patients
do after common procedures at our facility.
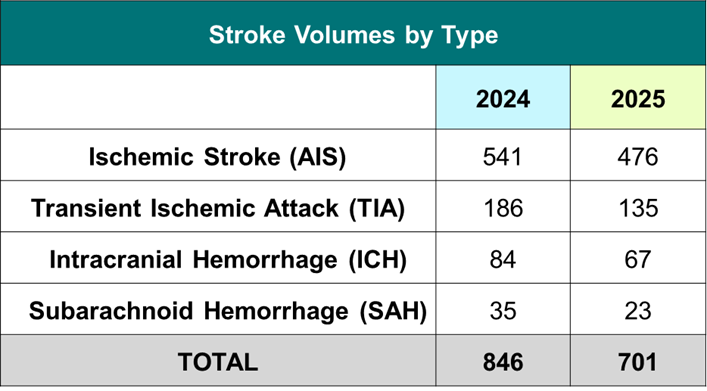
Stroke Program Volumes
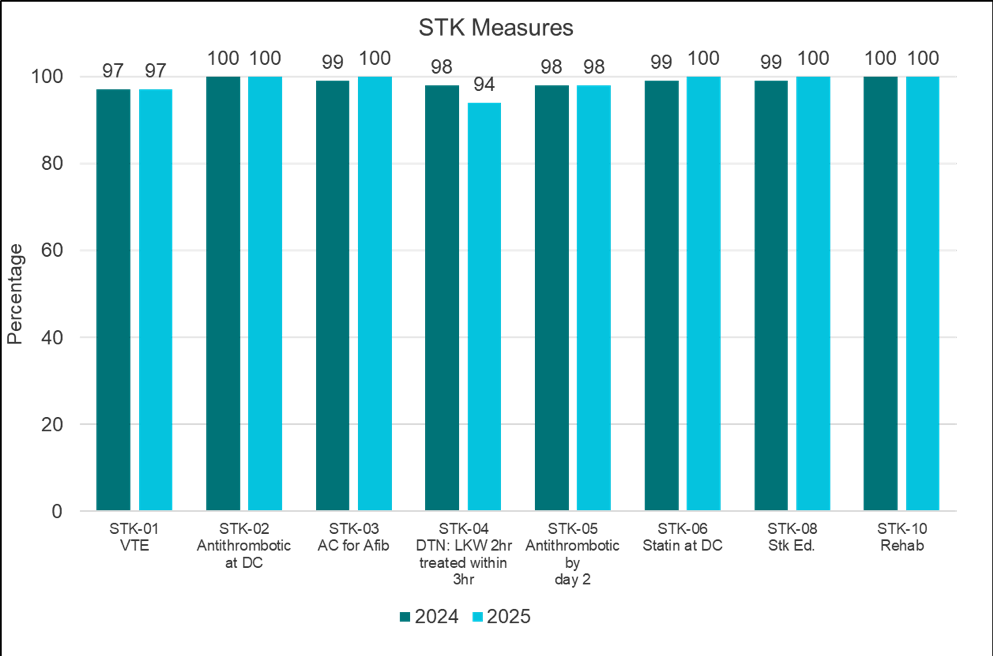
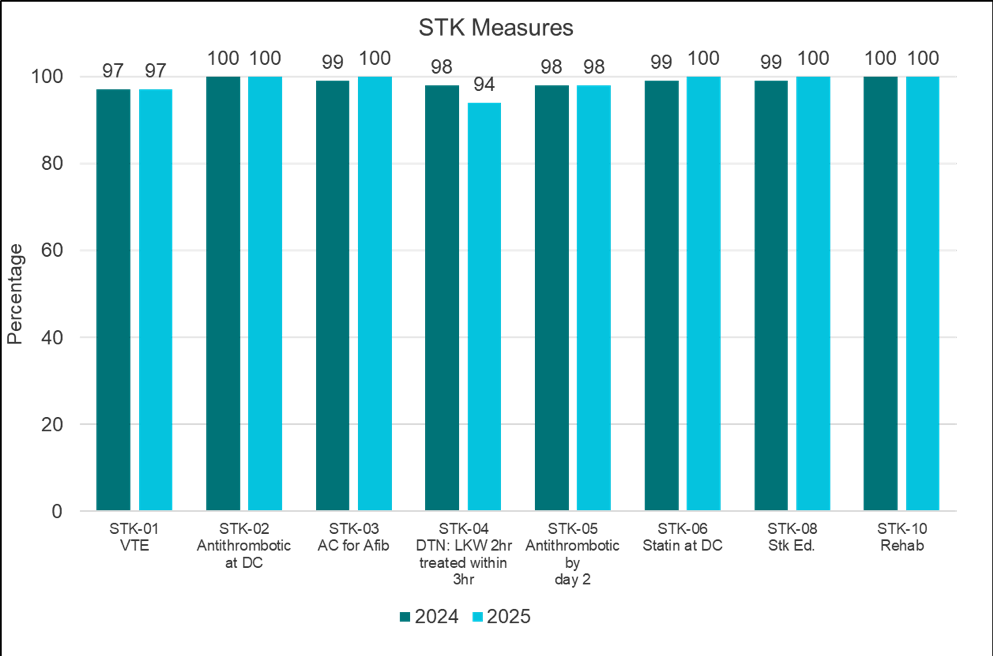
Stroke Quality Measures
CSTK-1: NIHSS in 12 hours
- All ischemic stroke patients will have an NIH Stroke Scale documented prior
to any intervention or within 12hrs of arrival.
STK-1: DVT Prophylaxis
- Ischemic and hemorrhagic stroke patients must receive VTE prophylaxis the
day of or day after admission
- Rationale: stroke patients are at an increased risk of developing a DVT
as opposed to other patients. A DVT (Deep Vein Thrombosis) is a blood clot.
STK-2: Antithrombotics prescribed at discharge
- Ischemic stroke patients must be discharged on an antithrombotic or if
the patient is ineligible for antithrombotic therapy, a reason must be
documented why.
- Rationale: data suggests that patients who take daily antithrombotic after
a stroke reduce morbidity and mortality.
STK-3: Anticoagulation for patients diagnosed with A-fib or A-flutter
- Ischemic stroke patients must be discharged on anticoagulant if presents
with afib/aflutter
- Rationale: these are risk factors for stroke. Prescribing an anticoagulant
at discharge helps prevent recurrence of stroke. If the patient is ineligible
for anticoagulation therapy, a reason must be documented why.
STK-4: Initiation of IV lytic (clot buster) within 3.5 hours of “last
seen well” for eligible patients
- IV lytic must be given within the applicable timeframe (if indicated)
- Rationale: IV lytic administration in eligible patients is most effective
if used within three hours of symptom onset. IV lytic is a medication
that helps break up the clot to restore blood flow to the brain.
STK-5: Antithrombotic therapy started at the end of hospital day no. 2
- Antithrombotics must be given by the end of hospital day 2 or documented
contraindication provided
- Rationale: studies show that administering an antithrombotic within two
days of stroke reduces morbidity and mortality.
STK-6: Patients should have an LDL level drawn within 48 hours of admission.
Patients with LDL >100 should be discharged home on Statin therapy
- LDL level must be drawn for all strokes within 48 hours of arrival
- Rationale: Patients with LDL > 100 mg/dL should be prescribed a Statin
at discharge to reduce the recurrence of stroke. High cholesterol is a
risk factor for stroke.
STK-8: Patients or family members must be provided with stroke education.
- Stroke education
- Rationale: Patients with strokes must be educated on risk factors, activation
of EMS, the importance of follow-up after discharge, medications they
have been prescribed, and warning symptoms/signs of stroke. Early activation
of EMS and proper treatment of stroke significantly increases life spans
of patients with stroke. Appropriate education is imperative to the reduction
of morbidity and mortality.
STK-10: Rehab must be considered for all patients
- Patient must be assessed for rehab services
- Rationale: two-thirds of people that suffer strokes every year survive,
leaving approximately 40% with some form of functional impairment. These
patients require some form of rehab.
National Benchmark Goal is 90%
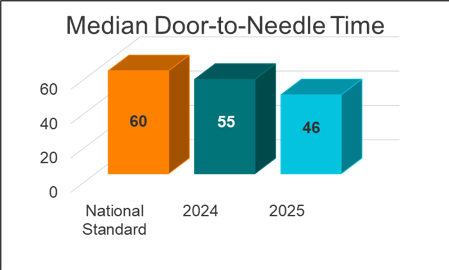
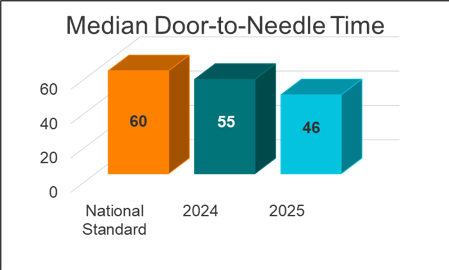
Door-to-Needle (DTN)/Clot busting medication
Median number of minutes from time of arrival at EJGH to start of treatment
with clot busting medication:
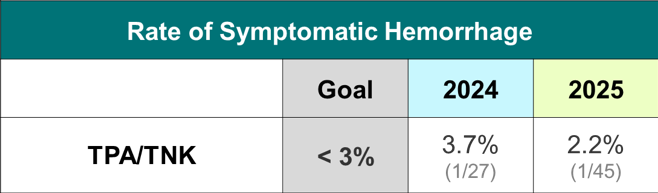
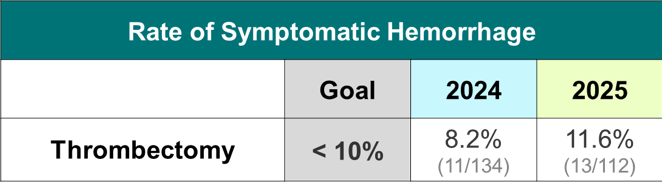
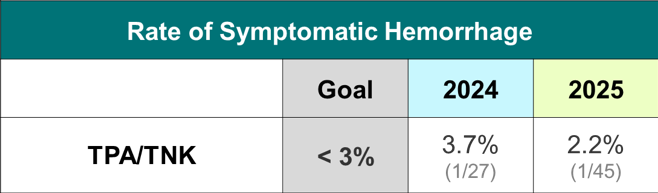
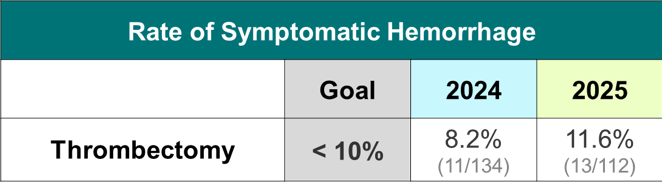
Percentage of patients with significant bleeding in the brain following
treatment with clot busting medication:
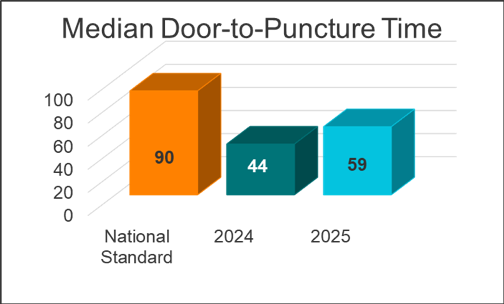
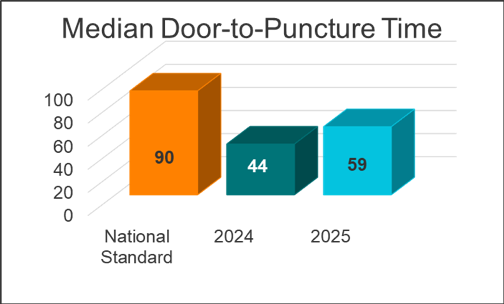
Door-to-Puncture(DTP)/Thrombectomy to remove clot
Median number of minutes from time of arrival at EJGH to start of treatment
with thrombectomy:
Percentage of patients with significant bleeding in the brain following
a thrombectomy procedure:
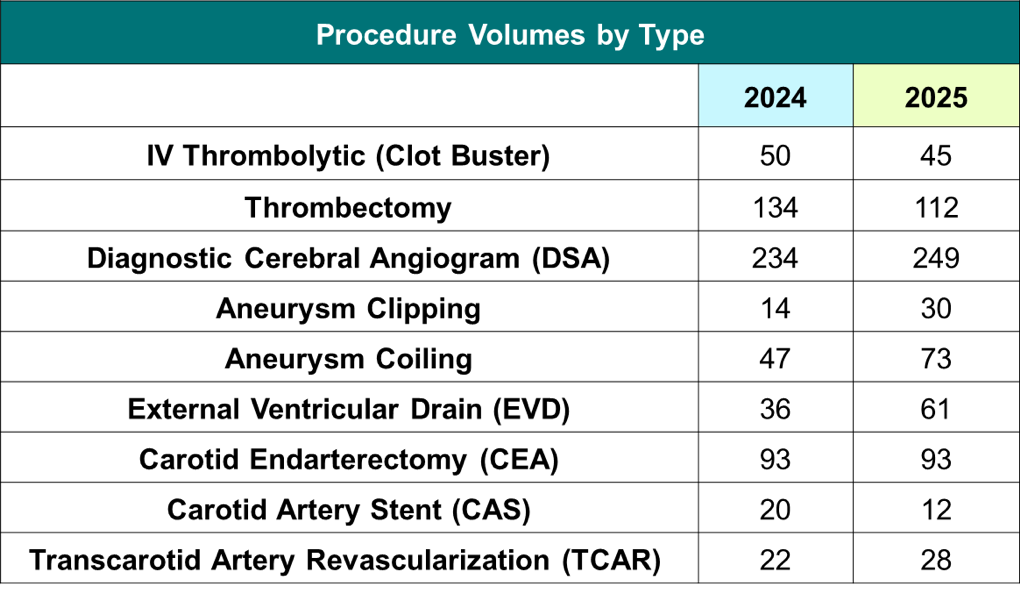
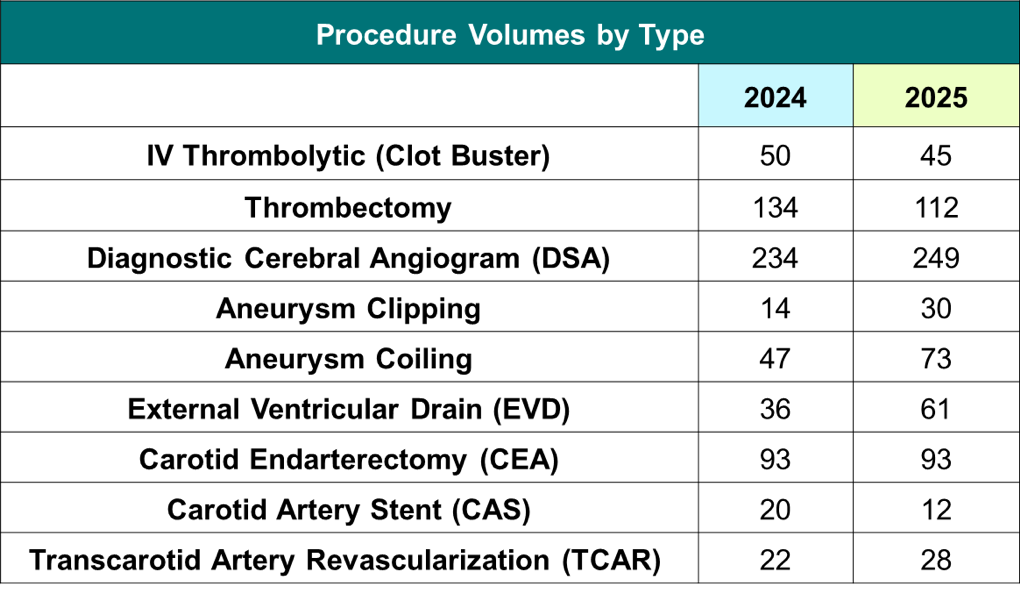
Common Procedure Definitions and Volumes
Neuroendovascular coiling of aneurysms
This procedure is used to treat aneurysms that may cause hemorrhagic strokes.
During the procedure, the doctor inserts a catheter into a blood vessel
located in the groin or in the wrist. The catheter is advanced through
the blood vessels into the brain where the aneurysm is located. The physician
will use the catheter to place many tiny metal coils inside the aneurysm.
The goal is to fill the aneurysm completely full of coils so it will not
rupture and bleed. This procedure does not require open surgery into the brain.
Microsurgical neurovascular clipping of aneurysms
This procedure is an open surgery to treat aneurysms that cause hemorrhagic
strokes. A neurosurgeon creates an opening into the skull to access the
brain where the aneurysm is located. The surgeon then places a small metal
clip on the blood vessel at the place where the aneurysm has formed. This
permanently cuts off the blood flow into the aneurysm. The metal clip
remains inside the brain after surgery.
Thrombolytic therapy ("clot busters")
Powerful medications, called thrombolytics, are used to treat ischemic
strokes by breaking up clots to get blood flowing again in that part of
the brain. The medicine may or may not completely break up the clot or
clots. The sooner these medications get to work, the more brain tissue
may be preserved, and less long-term damage may occur. They can only be
given within a short window of time after a person first notices symptoms.
Thrombectomy
This procedure is used in the treatment of ischemic strokes. During the
procedure, the doctor inserts a catheter into a blood vessel located in
the groin or in the wrist. The catheter is advanced through blood vessels
into the brain where the doctor will try to remove a blood clot located
in a large vessel in either in your neck and/or head to improve blood
flow to your brain.
Diagnostic Cerebral Angiogram
This is a minimally invasive surgery that uses catheters (endovascular)
to inject die into the vessels in the brain to see any possible aneurysms,
blockages, or narrow areas that may limit blood flow.
Carotid Endarterectomy (CEA)
This is a surgical procedure to remove the plaque—a hard, sticky
buildup inside the carotid artery that can block blood flow to the brain—
After the plaque is taken out, the artery is closed using stitches or
a small patch to help it heal.
This surgery helps lower the risk of stroke by making it easier for blood
to flow to the brain.
Carotid Artery Stent (CAS)
This is a minimally invasive surgery that involves placing a small mental
coil (stent) into a narrowed section of the carotid artery to help improve
blood flow and reduce the risk of stroke.
Transcarotid Artery Revascularization (TCAR)
This is a minimally invasive surgery that uses surgical balloons and small
metal coils (stents) to reopen a clogged or narrowed carotid artery to
help improve blood flow and reduce the risk of stroke.
External Ventricular Drain (EVD)
Your brain makes a special liquid called cerebrospinal fluid (CSF), which
helps protect it. But sometimes, too much of this fluid builds up, and
that can cause pressure inside the head. To fix this, doctors carefully
place a small tube into the brain to let the extra fluid drain out into
a bag outside the body. This helps keep the pressure in the brain at a
safe level and can also remove infected fluid if needed
Procedural Complication Rates
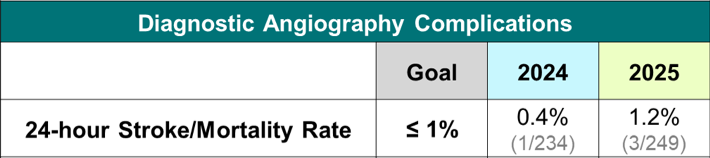
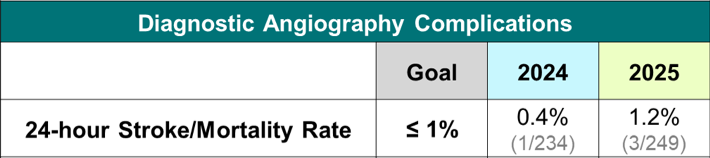
Diagnostic Cerebral Angiogram
Percentage of patients who experienced stroke or death within 24hrs of
the procedure:
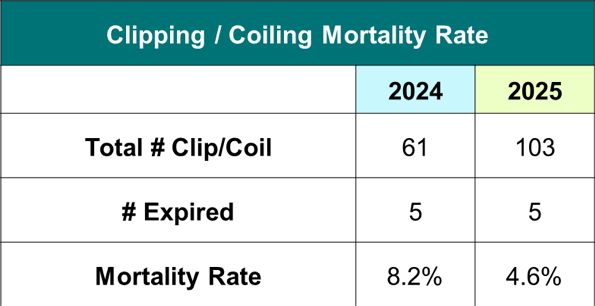
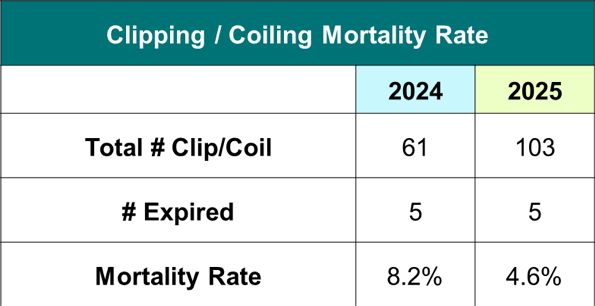
Aneurysm Procedures
Clipping/Coiling Mortality Rate:
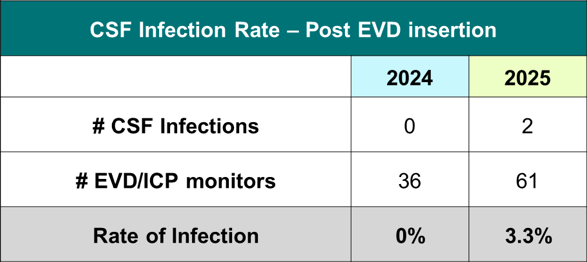
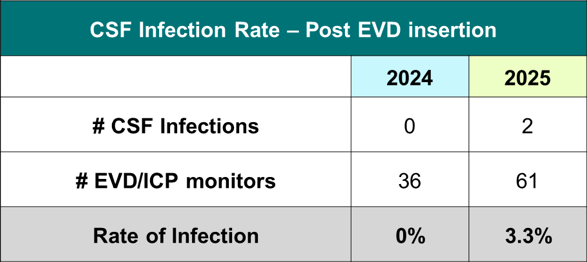
EVD Infection Rates
We monitor all patients that have an EVD placed for CSF infections related
to placement of the drain.
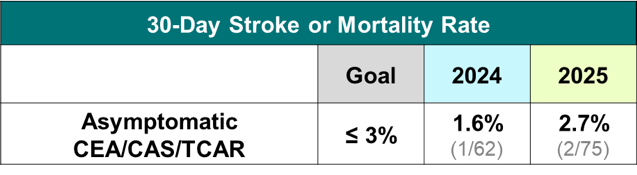
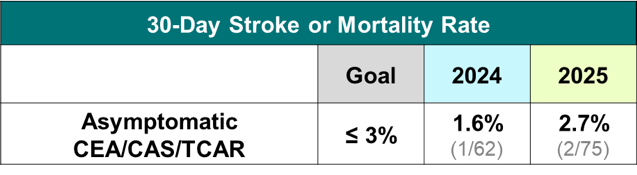
Asymptomatic Carotid Procedures
Percentage of patients who did not have symptoms prior to their procedure
and experienced stroke or death in the 30 days following their CEA/CAS/TCAR:
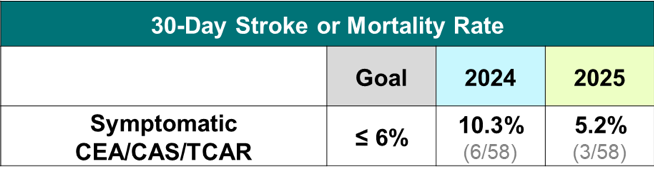
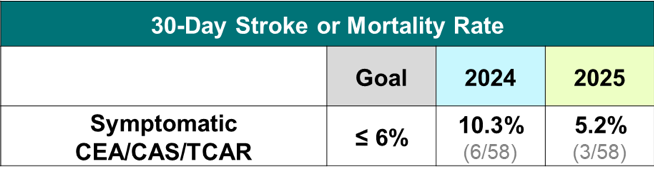
Symptomatic Carotid Procedures
Percentage of patients who did have symptoms prior to their procedure and
experienced stroke or death in the 30 days following their CEA/CAS/TCAR:
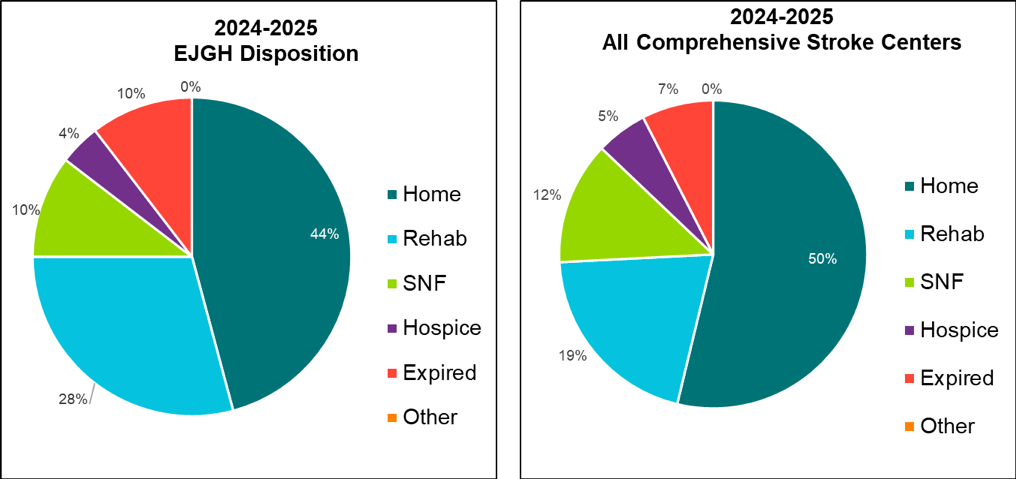
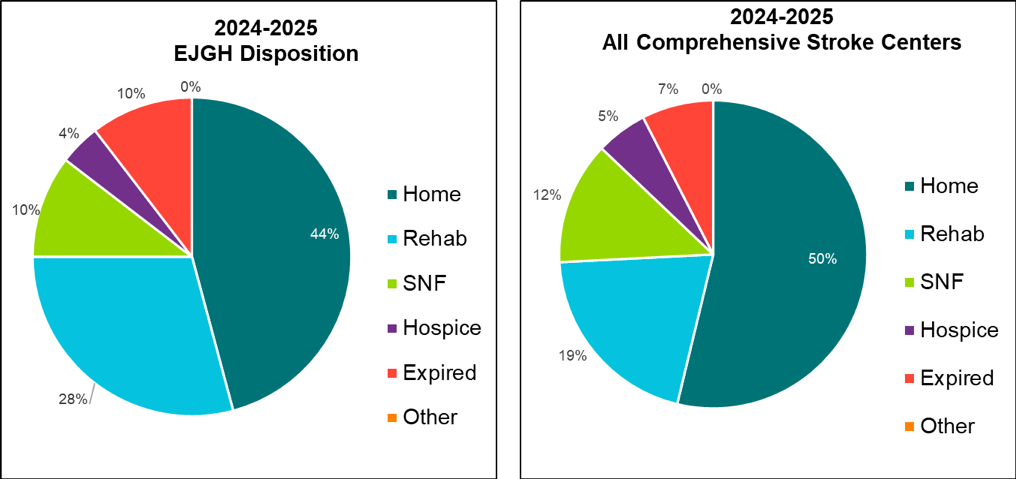
Discharge Dispositions